CONTACT
We will reply as soon as possible.
Enevia Health, LLC
30 N Gould Ste N, Sheridan, WY 82801, USA
Sources:
Infections and brain development – PMC (nih.gov)
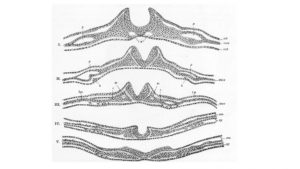
Human brain development and maturation occur throughout the fetal period and are modulated by a set of complex interactions between various signaling receptors, genetic/epigenetic factors, and environmental influences. The main stages of development during the gestational period are the following: primary neurulation (weeks 3-4), forebrain development (months 2-3), neuronal proliferation (months 3-4), neuronal migration (months 3-5), organization neuronal (postnatal period of 5 months) and myelination.
For example, abnormalities in primary neurulation can lead to neural tube defects, while abnormalities in neuronal organization can lead to mental retardation. The primary goal of this article is to examine the role that infection and inflammation play in fetal brain damage and impairment of neurocognitive function later in life.
Multiple epidemiological and retrospective studies carried out by the Department of Neuroscience and Cell Biology at Osaka University, Japan, have demonstrated an association between maternal infections, generally defined, and the development of cognitive and psychiatric diseases in offspring.
Despite the significant public health focus on autism, few in the scientific community realize its possible origins in intrauterine infection (IUI), although the existing evidence is weak. In a study of the Danish Medical Birth Registry from January 1980 to December 2005, more than 1.6 million births were registered for maternal prenatal admission for an infectious disease. 266 mothers (0.7%) were admitted for some type of infection, and 156 of the neonates born to these mothers were diagnosed with autism spectrum disorders (ASD) in psychiatric follow-up.
This study is particularly useful because it followed a large number of patients and reported on diagnoses made by trained clinicians, theoretically adding objectivity to the reporting of exposure and outcomes in this cohort.
The implication is that intrauterine infection may cause vulnerability in the fetal brain environment that may cause susceptibility to the later onset of psychiatric or neurodevelopmental disease.
Another very concrete way the data supports the link between infection and brain damage is through certain anatomical abnormalities observed in the brains of individuals infected with certain bacteria and viruses. However, it is important to note that these findings are not necessarily specific to intrauterine infection and fetal brain effects, making these associations tenuous at best.
We can mention cytomegalovirus (CMV) infections that are associated with pseudocysts, microcephaly, subependymal cysts, ventriculomegaly, cerebellar hypoplasia, hypoplastic corpus callosum, lissencephaly and polymicrogyria, and periventricular calcifications leading to necrosis and calcifications.
Although both primary maternal infection and CMV reactivation in pregnancy can cause fetal infection, approximately 10% to 20% of newborns born to mothers who have primary CMV infection have neurodevelopmental delays and sensorineural hearing loss. in the childhood.
Other viruses that cause brain inflammation are enteroviruses, which are associated with hydrocephalus; and lymphocytic choriomeningitis virus can cause various abnormalities in brain structure, such as microcephaly, periventricular calcifications, pachygyria, cysts and hydrocephalus, as well as structural and functional abnormalities of the eye.
Infections activate inflammatory pathways, causing the release of various proinflammatory biomarkers such as cytokines, interleukins, among other molecules. This inflammatory response can be measured in the context of pregnancy through:
All of these indicators of infection and inflammatory processes have also been associated with adverse neurological outcomes. Such studies provide further evidence for the theory that maternal infection during pregnancy may result in inflammation/infection-mediated fetal brain damage and thus potentially alter cognitive and psychological function later in life.
Cytokines are molecules produced by cells involved in the inflammatory pathway. They act by modulating the immune response by binding to receptors and causing the release of additional cytokines in a cascade-like mechanism.
Proinflammatory cytokines can cause direct damage to oligodendrocytes and neurons through activation of microglial cells, neurotoxicity, and neurobehavioral abnormalities.
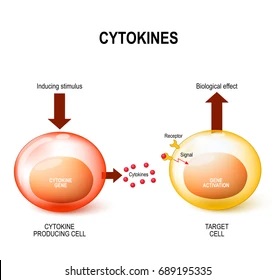
One of the most studied cytokines in the context of maternal infection and brain development is the proinflammatory cytokine, IL-6. Interleukin-6 is involved in the survival of several neurons, including acetylcholinesterase-positive, catecholaminergic, cholinergic, and dopaminergic neurons. It has also been shown that IL-6 can affect the electrical mechanism by which Purkinje and the enteric neuron function.
In inflammation, elevations of IL-6, IL-8, and TNF-[alpha] correlate with the development of cerebral palsy (CP) and schizophrenia and autism. Furthermore, other studies have shown that neonates with systemic fetal inflammatory response have elevated levels of IL-6 and suggested that IL-6 is an independent risk factor for severe neonatal morbidity.
With respect to schizophrenia, higher levels of the cytokine IL-8, measured in maternal blood during the second trimester, are predictive of the presence of schizophrenia spectrum disorders in a nested case-control study.
Specifically, in a sample of 59 mothers with 105 matched comparison samples for each category of schizophrenia spectrum disorder, the average level of IL-8 was found to be almost twice that measured in mothers whose children did not develop schizophrenia. .
A study was conducted where it was reported that individuals with a diagnosis of schizophrenia who had prior exposure to elevated serum levels of maternal IL-8 in utero had increased ventricular cerebrospinal fluid volumes, decreased left entorhinal cortex volumes, and decreased left entorhinal cortex volumes. and decreased right posterior cingulate volumes.

Of course, much more research is needed to understand the cytokine response during pregnancy and its possible subsequent effects on the fetal brain, because the existing evidence is not specific for associating fetal brain injury and maternal infection.
Chorioamnionitis is another active infection process that can affect neurodevelopment, within the amniotic cavity that can also induce a fetal inflammatory response and affects up to 10% pregnancies. The hypothesis is the overwhelming fetal production of cytokines that leads, among other organs, to brain cell damage.
The inflammatory process underlying maternal IUI is the quintessential mechanism of a significant portion of perinatal brain injuries and one of the main risk factors for neonatal sepsis. Studies investigating the pathogenesis of the sepsis cascade have revealed that IL-1[beta] is the biomarker that mediates brain injury in utero. The first causes the coagulation cascade, the recruitment of other interleukins and the activation of T cells.
Autism spectrum disorder is a heterogeneous neurodevelopmental disorder (NDD) that causes widespread abnormalities in social communication, repetitive behaviors, and restricted interests.
The prevalence of ASD is 1 in 44 (2,27%) patients in the US. The prevalence ratio of ASD among males and females has been reported to be 4:1. Although early interventions for ASD have been reported to improve symptoms, these interventions rely on symptomatic treatments, such as cognitive behavioral therapy.
In the prenatal setting, maternal immune activation (MIA), stress, drug exposure, and malnutrition are well-known environmental factors that affect offspring health. These environmental factors are highly associated with several NDD and psychiatric disorders, including ASD, attention deficit hyperactivity disorder (ADHD), schizophrenia, and depression.
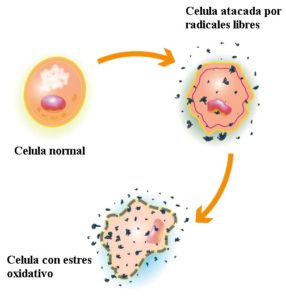
Oxidative stress is a phenomenon that damages cells and other organs by producing free radicals and peroxides due to a disorder of the redox state, that is, an imbalance of this state generates more oxidation within our body. Studies report that preventing these infection states generates 12% to 17% possibilities of reducing the incidence of ASD.
MIA is also known to deregulate genes associated with ASD and neurodevelopment. For example, MIA downregulates genes involved in axonal guidance, neurogenesis, and cytoskeleton, while upregulates genes involved in translation, cell cycle, and DNA damage. The activation of these genes can generate the appearance of symptoms that are associated with ASD.
In animal studies, MIA induced by lipopolysaccharides similar to those found in gram-negative bacteria has been reported to cause acute vascular damage in the placenta, along with transient hypoxia and reduced proliferation of neural progenitor cells in the developing mouse embryonic brain. .
Furthermore, reduced numbers of SATB2-, PV-, and TBR1-positive cells have also been reported in the cortex of embryos from the mother suffering from LPS-induced MIA, indicating abnormalities in cortical lamina and connectivity in the offspring. of MIA mice.
As the placenta is affected by inflammatory cytokines induced by MIA, the inflammation causes placental necrosis and loss of potential growth or possibilities of intrauterine growth restriction. Depending on the severity of placental insufficiency it will be the symptoms of the fetus or the symptoms of the individual in his life.
It should be noted that the same deterioration of the placental barrier causes deficiency in the contribution or supply of nutrients to the fetus. In addition, the function of the placental barrier is similar to that of the blood-brain barrier, so all blood components pass from the mother to the child without any filter.
The placental barrier exists for a reason and that is to protect the fetus. The blood-brain barrier of the fetus itself, being not mature but just in formation, is susceptible. By containing maternal inflammatory cytokines, they will produce oxidative stress and antibodies, in the critical stages of fetal development where this immature blood-brain barrier exists, a brain in just formation.
The human body has a limited way of functioning, in regards to infections, stress and inflammation, being subjected to these circumstances does not develop or grow properly, since all the energy will be directed towards coping with the situation of cellular stress in which is affected.
Inflammation-induced cell death in the fetal brain and oxidative stress substantially influence fetal brain development. In the same way it works in the first three years of life, any external or internal agent that can generate cellular stress will inhibit its correct development and will depend on the causal agent of the damage, since both in the first stages of the gestational period and in the development of the nervous system as well as after birth, when the brain is more plastic to changes and regeneration.

After the first years of life, the cells tend to behave more like adult cells, their regeneration and response period will decrease. Therefore, care from an early age, gestational or not preconception, can establish significant benefits for the prevention of many neurodevelopmental diseases.
However, many aspects related to the effects of neuroinflammation on brain development on the pathogenesis of ASD remain unclear. The involvement of neuroinflammation in the pathogenesis of PDD has recently been discussed in both clinical and basic research fields, and it has been suggested that neuroinflammation is important not only in ASD but also in other ADD, such as ADHD.
In mouse studies similar to those we mentioned above, MIA has been reported to induce the expression of the ROS-producing enzyme NADPH oxidase 1 (Nox1) in the fetal brain, leading to ASD-like behaviors and reductions in TBR1-positive layer 6 neurons in the mouse cortex and Purkinje cells in the mouse cerebellum.
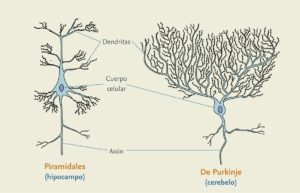
Purkinje cells send inhibitory projections to the deep cerebellar nucleus, and constitute the only outlet for all motor coordination in the cerebral cortex. Its associated neurotransmitter is GABA, so damage to these cells will include a decrease in said neurotransmitter in those areas.
Being one of the largest nerve cells, added to the characteristics of their histology, their regeneration is not possible, added to the fact that they are very susceptible to poisoning by toxic substances such as Lithium, autoimmune diseases and mutations that lead to neurodegenerative, neurodevelopmental or other diseases. ataxias.
The 40% of ataxias of unknown origin are due to Gluten consumption, and are the 15% of all ataxias. It can appear in people of all ages, including children. It is an autoimmune disease caused by the consumption of gluten, classified into the so-called gluten-related disorders, with or without intestinal involvement, that is, it may or may not be celiac. Which explains to us once again the importance of the brain-gut axis.
The complicated thing is that the death of the cerebellar neurons is the result of prolonged exposure to the harmful agent, which is irreversible. As always, early diagnosis and early treatment with a gluten-free diet allow stabilization and even complete recovery. If the diagnosis is made late, when considerable destruction of neurons has already occurred, dietary restriction to gluten does not provide us with greater benefit than avoiding further damage; Therefore, certain laboratory tests are very important to understand how we function.
The key to success is prevention, starting with knowing maternal health since the mother can make immune responses. It is also important to know the genetics of the parents. Pregnancy planning is crucial for correct pregnancy control in each of the trimesters. The study of amniotic fluid helps us determine many chromosomopathies. Neonatal screening is crucial to prevent damage and treat many diseases in time. allergens, autoimmunity and environmental poisoning are very important. Some will require annual controls, others once is enough.
Prevention is always the key to success, the regeneration of our body is finite, and we can reach irreversible states if we do not treat them in time, and the time it takes to observe the symptoms covers the first 3 years of life and can be irreversible if We don't know our genetics or we don't keep good control of our children's health.
Knowing the stages of our children's neurodevelopment is crucial to prevent, diagnose and treat in time many diseases that can be preventable and reversible if treated in time.
Don't hesitate to go to your doctor, pediatrician, gynecologist, geneticist or immunologist in time! You can also make a consultation with one of our specialists through our website at:
Prevention is the key to your health!
We will reply as soon as possible.
30 N Gould Ste N, Sheridan, WY 82801, USA
Our groups are the ideal platform to learn and share your scientific concerns about neurodevelopment issues
*Our purpose is informational only, it is not intended to be a substitute for medical advice, diagnosis or treatment.
We are working on our website. For any queries, you can contact our customer service team at atencionalcliente@eneviahealth.com